Glossary: What is the Trachea
The trachea, commonly known as the windpipe, is a crucial part of the respiratory system. It serves as a passage for air to travel to and from the lungs, playing a vital role in maintaining healthy breathing. Understanding the trachea involves exploring its definition, anatomy, function, and relevance in both humans and other animals.
Understanding the Basics of the Trachea
Definition and Function of the Trachea
The trachea is a tube-like structure that extends from the larynx, which is located at the base of the throat, and branches into the two primary bronchi leading into the lungs. Its primary function is to ensure that air can move freely in and out of the lungs. The trachea is lined with a mucous membrane that helps to trap dust, pathogens, and other particles found in the air we breathe.
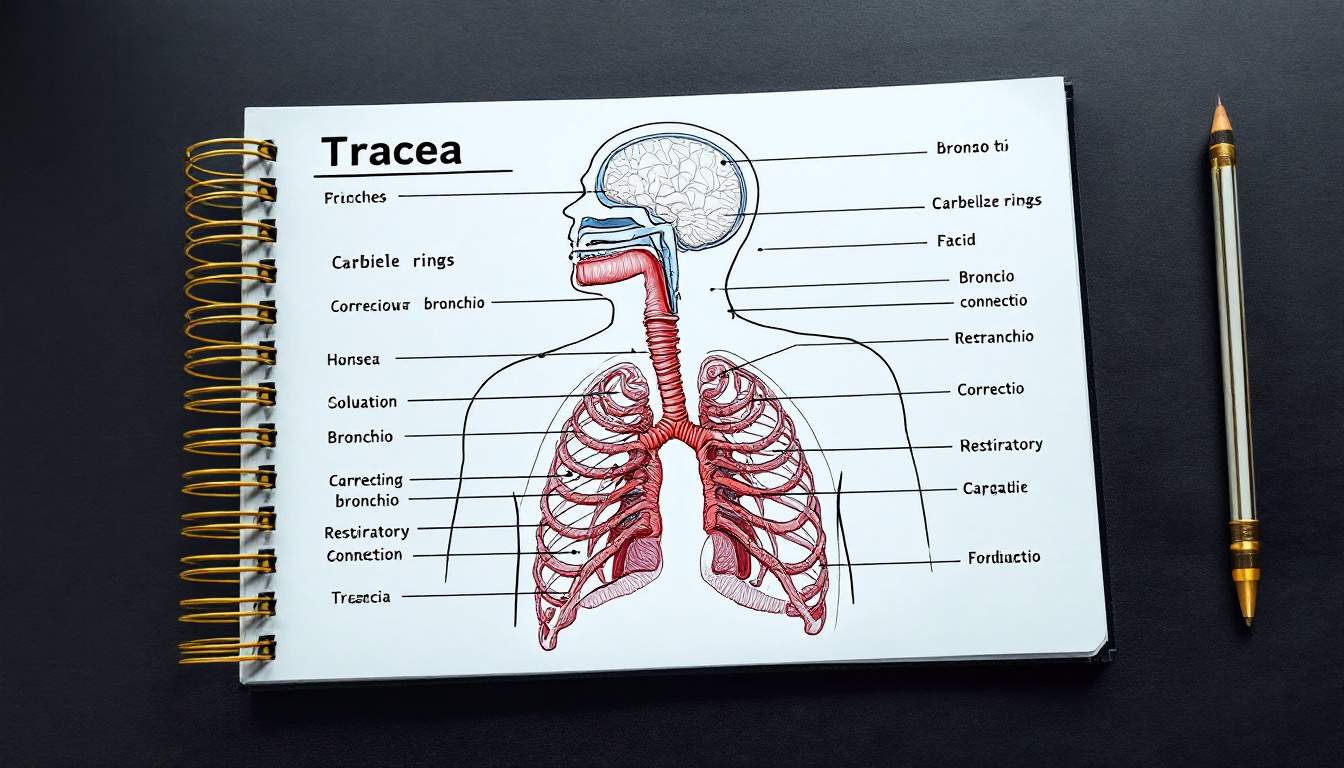
Moreover, the trachea is a rigid structure supported by C-shaped cartilage rings. These rings prevent the trachea from collapsing and maintain an open airway, allowing for uninterrupted airflow during inhalation and exhalation. The flexibility of the trachea is also crucial, as it allows for movement during swallowing and other activities that involve the neck and throat, ensuring that the airway remains unobstructed.
Anatomy of the Trachea
Anatomically, the trachea is about 10 to 12 centimeters long in adults and has a diameter of around 2 to 2.5 centimeters. It is comprised of several layers: the innermost mucosa, a layer of cartilage, and an outer layer known as the adventitia. The mucosa is lined with specialized cells that produce mucus and cilia, tiny hair-like structures that help move trapped particles out of the respiratory tract. This mucociliary escalator mechanism plays a vital role in keeping the airways clear and free from irritants, contributing significantly to respiratory health.
The trachea splits into two main bronchi at a site known as the carina, which is located at approximately the level of the fifth thoracic vertebra. The right bronchus is wider and more vertically oriented than the left, making it more prone to aspirated objects. This anatomical difference is particularly important in medical settings, as it influences the likelihood of foreign body aspiration and the approach taken during bronchoscopy procedures. Understanding these nuances can aid healthcare professionals in diagnosing and treating respiratory issues effectively.
The Role of Trachea in the Respiratory System
Trachea's Connection with Lungs
The trachea serves as a significant connection point between the upper respiratory tract, including the throat and nasal passages, and the lungs. When you inhale, air travels through the nasal passages or mouth, directs through the larynx, and then enters the trachea. From there, it continues into the bronchi and eventually reaches the alveoli, where gas exchange occurs.
This connection is vital as it allows for the efficient transfer of oxygen into the bloodstream and the removal of carbon dioxide, a waste product of metabolism, from the body during exhalation. The trachea itself is a flexible tube made of cartilage rings, which not only keeps it open but also allows for slight movements during breathing and swallowing. This structural design is essential for maintaining airflow while also accommodating the movements of the neck and chest during respiration.
How Trachea Facilitates Breathing
The trachea not only functions as a conduit for air but also plays a role in the humidification and warming of the air that enters the lungs. This is critical, particularly in colder climates or during strenuous exercise when air is inhaled more rapidly and in larger volumes. The lining of the trachea contains mucus-producing goblet cells that trap dust, pathogens, and other particles, ensuring that the air reaching the lungs is as clean as possible.
Additionally, the trachea's cilia move in a coordinated manner to push mucus upwards towards the throat, helping to clear out irritants and infectious agents. This process is an essential part of the body’s defense mechanism against respiratory infections and pollution. Furthermore, the trachea has sensory nerve endings that can trigger a cough reflex when irritants are detected, providing an immediate response to protect the lower respiratory tract. This reflex is crucial for preventing potential obstructions and maintaining clear airways, showcasing the trachea's multifaceted role in respiratory health.
Disorders and Diseases of the Trachea
Common Tracheal Disorders
Several disorders can affect the trachea, ranging from infections to structural abnormalities. Common conditions include tracheitis, which is an inflammation of the trachea often caused by a viral infection, and tracheal stenosis, which is the narrowing of the trachea due to various reasons, including injury or congenital defects.
- Tracheomalacia: A condition where the tracheal walls become too soft, leading to collapse, particularly during breathing.
- Foreign Body Aspiration: When an object gets lodged in the trachea, risking suffocation and requiring immediate medical attention.
- Tracheal Tumors: Abnormal growths that can obstruct airflow.
Symptoms and Diagnosis of Tracheal Diseases
Symptoms of tracheal disorders can vary, but common signs include coughing, wheezing, difficulty breathing, and a version of stridor, which is a wheezing sound that indicates turbulent airflow. Diagnosis typically involves a combination of physical examinations, imaging studies like X-rays or CT scans, and sometimes endoscopy.
Early detection is critical, as untreated tracheal conditions can lead to severe respiratory complications. Healthcare professionals employ various diagnostic tools tailored to the individual's symptoms and medical history to arrive at an accurate conclusion. For instance, a bronchoscopy may be performed to visualize the trachea directly, allowing for a more detailed assessment of any abnormalities or blockages. This procedure can also facilitate the removal of foreign bodies or the collection of tissue samples for further analysis.
In addition to the physical symptoms, patients may experience psychological distress due to the chronic nature of some tracheal disorders. The fear of suffocation or the anxiety surrounding breathing difficulties can significantly impact a patient's quality of life. Support groups and counseling may be beneficial for those coping with the emotional toll of these conditions, providing a platform for sharing experiences and strategies for managing symptoms effectively.
Treatment and Management of Tracheal Conditions
Medical Interventions for Tracheal Diseases
Treatment of tracheal issues often depends on the specific diagnosis. For infections, such as tracheitis, antiviral medications may be prescribed along with supportive care, such as humidified air to ease breathing discomfort. In some cases, corticosteroids may also be utilized to reduce inflammation and swelling in the trachea, allowing for improved airflow and relief from symptoms.
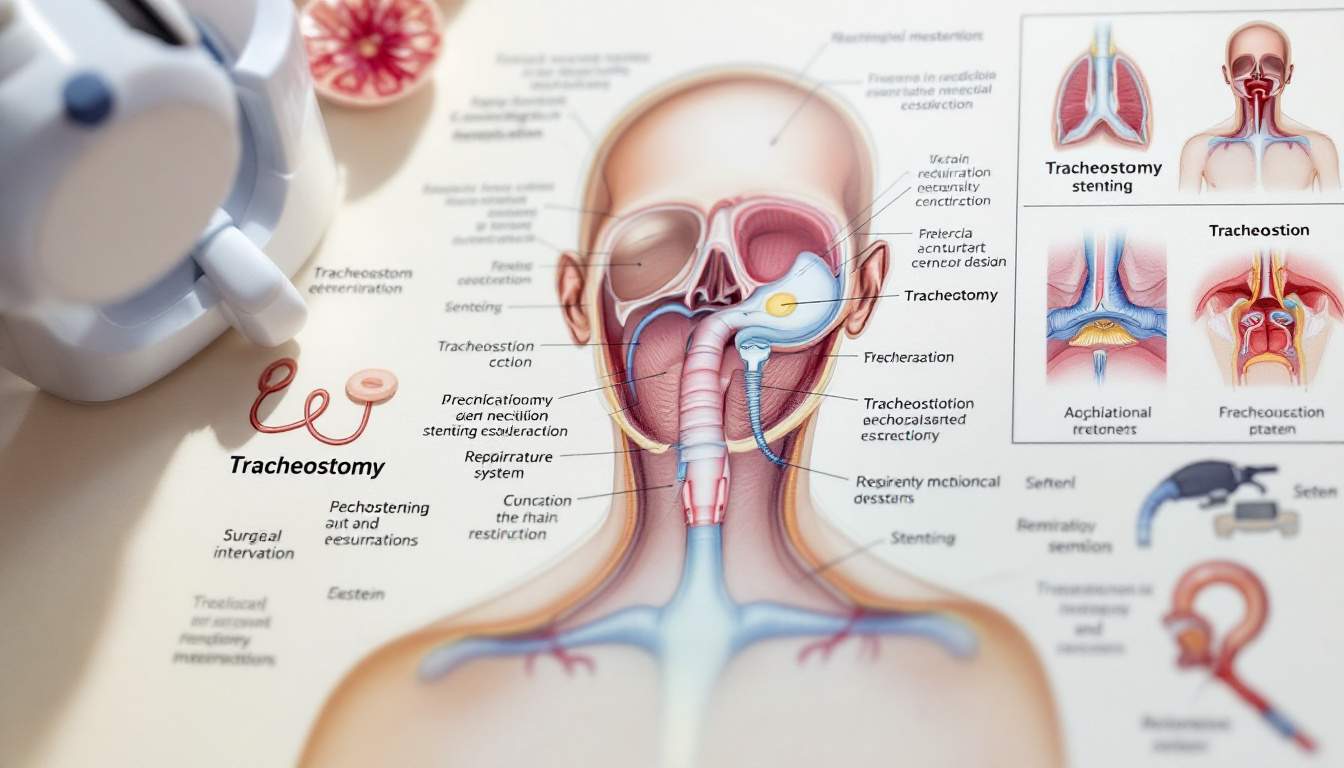
In cases of structural issues like tracheomalacia or stenosis, more invasive procedures may be necessary, including tracheoplasty or the insertion of stents to keep the airway open. Serious cases may require surgical intervention or tracheostomy, where an opening is created in the neck for breathing. Post-operative care is crucial, as patients may need to be monitored for complications such as infection or airway obstruction. Rehabilitation programs can also play a vital role in helping patients regain their strength and lung function after such procedures.
Lifestyle Changes for Tracheal Health
Alongside medical interventions, adopting healthy lifestyle changes can significantly improve tracheal and overall respiratory health. Staying away from smoking and secondhand smoke, staying hydrated to help maintain optimal mucus production, and engaging in regular exercise can be beneficial. Additionally, practicing good hand hygiene and avoiding close contact with individuals who are ill can help reduce the risk of respiratory infections.
- Regular Healthcare Check-ups: Regular visits to healthcare professionals can aid in early detection and management of potential issues. These check-ups can also provide opportunities for vaccinations, such as the flu shot, which can help protect against respiratory illnesses.
- Allergy Management: Identifying and managing allergies can prevent inflammation and irritation in the airways. Utilizing air purifiers, keeping windows closed during high pollen seasons, and regularly cleaning living spaces can significantly reduce allergen exposure.
- Healthy Diet: A balanced diet rich in vitamins and antioxidants supports immune function, which can be beneficial for respiratory health. Foods high in omega-3 fatty acids, such as fish and walnuts, can also help reduce inflammation in the body, further supporting tracheal health.
In conclusion, the trachea is a vital component of the respiratory system. A deeper understanding of its structure, function, and relevance in health and disease highlights the importance of maintaining its integrity for optimal respiratory health.
Understanding the intricacies of the trachea and its role in respiratory health is just the beginning. With Alveo's innovative Continuous Respiratory Wearable, you can take your knowledge to the next level by monitoring your respiratory system in real-time. Experience the comfort and ease of personalized breathing routines, gain insights into how your environment affects your breathing, and stay alert with real-time monitoring. Ready to breathe smarter and live better? Sign up on our waiting list today and be among the first to embrace the future of respiratory health with Alveo.